June is Lipedema Awareness Month – I’m sharing my story to help raise awareness.
In my previous post, I shared my diagnosis of Lipedema Stage 1, Type 3 & 4, along with other conditions such as FLM, and she suspects EDS, and Veinous Insufficiency.
After receiving the diagnosis, my husband and I decided to continue IVF to expand our family. This time, we opted for a donor egg to prevent our child from inheriting my challenging genetic conditions. It also allowed me to avoid the hormone drugs used in the egg retrieval process, which had previously caused significant swelling and fatigue.
Knowing that pregnancy can trigger Lipedema, I was determined to manage its progression through careful diet management, wearing compression garments, engaging in regular walking, and swimming at the local pool. Despite my previous painful pregnancy experience, I believed that I had identified the source of my discomfort and hoped for a smoother journey this time.
To prevent the hip pain, I had experienced during my previous pregnancy, I began physical therapy. I attended sessions twice a week, focusing on strengthening my hips. Additionally, I made it a habit to visit the pool three or more days a week and daily walk to get my kids from school. Then Covid hit.
During my pregnancy, I made a conscious effort to avoid nightshades in my diet. While my goal was to follow a low-carb eating plan, I developed a meat aversion and found myself craving cheese quesadillas, so I made them with almond flour to adhere to low carb. Overall, it was a relatively good pregnancy compared to my first, although I did struggle with some neck, back, and hip pain that my physical therapist addressed. We tried cupping to fix this pain, but it continued to come back.
I had two major issues occur during my pregnancy. One day I woke up with tons of skin tags that ran from my left armpit across my breasts. When I consulted with my doctor, she said pregnancy hormones do weird things to the body.
Later I learned that skin tags are a sign of insulin resistance. While my A1C was normal, I’ve since learned from other women with Lipedema, that you can still have insulin resistance with a normal A1C. Skin tags and another skin condition called, acanthosis nigricans are signs. Prior to this happening, I was only consuming about 15 grams of sugar a day in the form of honey, in addition, sometimes fruit like mandarin oranges and strawberries.
My family often goes for ice cream in the summer and once a year I partake. We go to a place that makes in house frozen custard, because it doesn’t have any added starch. Many ice-cream and gelato places add starch, which triggers my nightshade reaction. The skin tags occurred after this one indulgence. Eventually most the skin tags sloughed off, except the large ones, that I figured out how to remove. I’ve finally learned my body can’t tolerate any sugar indulgences. One indulgence is NOT worth it.
The most significant issue arose on the day I received the d-tap vaccine, which triggered severe neck and back pain, as well as uterine spasms when I stood for prolonged periods or when walking. As a result, I had to refrain from standing and walking for a month until the spasms subsided. I should have learned from my previous pregnancy experience.
Fortunately, I managed to avoid giving birth on the side of the road, after getting a flat tire while I was in labor, and in transition. I made it to the hospital just in time and I felt relatively good after delivery. However, approximately two weeks post-partum, I started experiencing intense pain in my hips.
Over the course of a few months, I discovered that I had developed a sensitivity to certain plant-based foods that were increasing the joint pain. Legumes were among the culprits, although there were others that proved challenging to identify. Unfortunately, I began losing mobility, and the pain became too severe to carry my baby around.
Given the level of pain I was enduring, I wasn’t able to exercise. I allowed some carbs in my diet, mostly sweet potato and almond flour products. I added these carbs to try to produce milk. I brought a vibration plate, and I resumed physical therapy after four months. Despite several months of physical therapy, my condition did not improve, prompting me to request imaging from my doctor. However, instead of supporting my request, my doctor suggested finding a new physical therapist. Frustrated, I turned to the internet for information and came across the heightened risk of labral tears in individuals with EDS who had gone through childbirth. I persisted in advocating for imaging on my hip.
Following an MRI, I was referred to an Orthopedic Surgeon who diagnosed me with Complex Labral Tear, Glute Tendinosis, Osteoarthritis, and minimal cartilage, all resulting from undiagnosed Hip Dysplasia. Consequently, I required a left total hip replacement. It was yet another genetic disorder that went unnoticed during my younger years and it explains why I couldn’t do squats. Hip Dysplasia means that the hip joint where the socket portion does not fully cover the ball portion of the upper thighbone the hip This causes rapid aging of the hip. This is one of the reasons why I feel like I’m 90 years old.
During this period, I relied on crutches for mobility and was unable to carry around my baby. Additionally, I experienced an excruciating amount of pain in my right foot. I was told it was just plantar fasciitis, but it felt much worse than PF. It didn’t matter what leg I put my weight on, it all hurt.
I visited a vein doctor in order to address Veinous Insufficiency. Given their specialization in women’s legs, I assumed they would be knowledgeable about Lipedema. Surprisingly, this doctor, who had also worked as an OB, and her staff repeatedly confused Lipedema with Lymphedema. Despite the confusion, they did confirm Dr. Herbst’s suspicion regarding Veinous Insufficiency. I had surgery scheduled to address my veins, but I had to cancel it in order to prioritize a different surgery that was crucial for restoring my mobility – a Left Total Hip Replacement.
I underwent hip replacement surgery when my baby was just 11 months old. I know what some of you are thinking. I should not have had a baby at age 44. I am actually glad I struggled with infertility. If I’d had my babies in my 20’s, it’s likely I would’ve needed a replacement much earlier in life. This would’ve also caused the Lipedema to progress much earlier. Replacements only last 20 years, I could be getting my replacement replaced at this age, if I’d had my babies in my 20’s. Infertility was a blessing in disguise.
While most people can begin walking with a hip replacement on the same day, utilizing a walker, my surgery did not go as smoothly. I was prohibited from putting any weight on my hip for five weeks, confining me to bed rest except for engaging in some physical therapy exercises. Despite my concerns about weight gain, I surprisingly lost 10 pounds during this time, leaving me with 20 pounds of baby weight to lose. I often wondered if any of the medications influenced this outcome, as I continued to eat the same low-carb diet, but I decreased my activity…. strange.
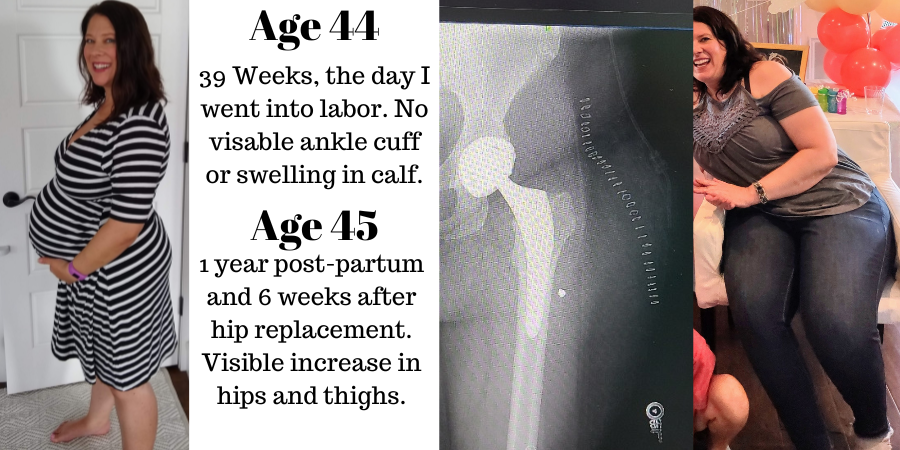
Once I regained the ability to move without the aid of walking aids, I hoped to shed the remaining baby weight by returning to the keto diet and exercising. I hadn’t gained any weight, but my thighs looked significantly bigger. However, I encountered difficulties with my right hip, which still has Hip Dysplasia. I started keto, but the weight was not budging.

In the FB Lipedema Communities, some of the women mentioned that keto didn’t work, but Carnivore worked really well for them. Intrigued by their success, I consulted with my doctor, who recommended that I continue consuming green vegetables.
I was burdened by a long list of health problems for which I found no relief. Gout, tennis elbow, severe dry eyes, unquenchable thirst despite consuming lots of water, kidney pain, dry skin, hypercalcemia, high DHEA, high testosterone, PMS, headaches, poor sleep, intermittent carpal tunnel syndrome, excruciating foot pain due to plantar fasciitis and diminished fat pad, mild depression, and an inability to lose weight were among the issues I faced. Both my new hip and my old hip caused me pain, and I continued to walk with a limp. The hip replacement side appeared visibly larger than the other, it was also painful to the touch, making it impossible to lie on my left side. I couldn’t help but wonder whether the hip replacement surgery had damaged my lymphatic system and if the Lipedema had progressed in my left hip.
I worried about the Lipedema advancing in my left hip, I attempted to secure a lymphatic pump through my insurance. Unfortunately, my request was denied, and the representative I spoke to insisted that I go on a diet first. WHAT!?
It was beyond frustrating to feel like I was doing everything right according to what I had been taught, yet still experienced debilitating pain and ALL these other symptoms. I felt much older than my years and questioned whether I deserved such a wonderful husband. I believed my children deserved a better mother who could embark on adventures with them. It felt as though my brain was betraying me, and I reached a point of surrender.
In my next article I’ll share what has been causing so much inflammation and what brought me relief.